Critical Review on the Contribution of Machine Learning to Health Science
DOI:
https://doi.org/10.62487/qgpcnt08Keywords:
Health Science, Healthcare, Machine Learning, Critical review, EvaluationAbstract
Background: The field of machine learning in health science is evolving exponentially, with a focus on accelerating scientific discoveries, improving holistic well-being, and advancing personalized healthcare. Aim: In this same spirit, this critical review article aims to provide a comprehensive understanding of the role, challenges, opportunities, and ethical considerations of integrating machine learning into health science, with an emphasis on healthcare research and practice. Methods: To base its critiques on previous literature, the elucidative survey considered specific criteria, such as the significance and contribution of each source to the field, methodology or approach, and argument, as well as the use of evidence. Results: The study results indicate that machine learning holds great promise to improve evidence-based health science, but significant work is needed to ensure the technology is developed and deployed in a way that is trustworthy and ethical. Conclusion: In conclusion, the literature review presents a balanced assessment of the strengths, weaknesses, and notable features of the current state of machine learning in health science. The key takeaway point is that while machine learning has demonstrated significant potential to improve health science outcomes and strategic management, there are still important challenges, limitations, and research gaps that need to be addressed to facilitate widespread adoption and trust in these technologies.
Introduction
Machine learning (ML) has brought significant changes to health science1. For instance, recent developments in the healthcare industry have demonstrated amazing growth and prospects to support doctors and enhance precision, prognosis, and care quality2. Moreover, ML attempted to help health science stakeholders improve decision-making and reduce risks in the medical and well-being fields. This critical review delves into the applications and challenges of machine learning in health science and, more particularly, in the healthcare domain3. It highlights the potential of ML to improve health science outcomes through predictive analytics, diagnosis and treatment, personalized medicine, clinical decision support, and population health management3. The review also discusses the ethical concerns and challenges associated with the use of ML in healthcare, including the risk of amplifying existing health inequities and the need for reproducible and interpretable models4 5. It underscores the importance of addressing barriers, fostering transdisciplinary collaboration, and optimizing scalable growth in high-impact collaborations between clinical researchers and ML experts to enhance clinical care through innovative technologies and methodologies.
Brief statement of the overall literature evaluation
The literature underscores the transformative potential of ML in healthcare, ranging from enhancing healthcare management to evaluating online health information quality. The systematic reviews provide valuable insights into the current state-of-the-art applications of ML in health science research, emphasizing the need for further research and development to leverage ML effectively in healthcare settings.
What is currently unknown in the field of machine learning in health sciences?
In the field of machine learning in health sciences, one of the current unknown aspects is the presence of "unknown unknowns." These are classes or categories of data that are not only unknown but are also unrecognized due to misperception or mislabeling within the training data. These unknown unknowns pose a significant challenge in conventional supervised learning, where models are trained on datasets with known labels. Addressing these unknown unknowns is crucial for enhancing the accuracy and reliability of machine learning models in healthcare applications. The concept of unknown unknowns in machine learning for health sciences refers to classes of data that are present but not identified or understood within the training dataset. Traditional methods of re-selecting algorithms or increasing training samples are insufficient to tackle this issue. To address the unknown unknowns, an approach called exploratory machine learning is proposed. This method allows the model to detect unsatisfactory learning performance and then augment the feature space to make these unknown classes observable for learning. This strategy aims to improve the model's ability to recognize and classify data that was previously unrecognized, enhancing the overall performance and reliability of machine learning models in healthcare applications. This challenge highlights the need for continued research and innovation in machine learning to uncover and address these unknown unknowns, ultimately improving the accuracy and effectiveness of machine learning applications in the field of health sciences.
Main thesis of this critical review
The main argument of this critical review is centered around the strengths and limitations of ML in the health science industry. The latter is praised for providing a robust framework for uncovering causal relationships and understanding the natural world. However, it is also acknowledged that ML is limited by the scope of human understanding, the ability to design and execute meaningful experiments, inherent biases in data, and the complexity of real-world problems.
Material and Methods
The methods of information collection for this critical review article encompass formulating research questions, searching the literature, screening for inclusion, assessing study quality, extracting, and analyzing data, and utilizing secondary data collection methods to ensure a thorough and well-rounded review process. Here are some key platforms searched for systematic reviews related to ML in health sciences:
1. PubMed - A comprehensive database of biomedical literature, including systematic reviews on ML applications in healthcare.
2. Cochrane Library - A collection of databases that contain high-quality, independent evidence to inform healthcare decision-making, including Cochrane systematic reviews.
3. Embase - A biomedical and pharmacological database that indexes systematic reviews and meta-analyses, including those on ML in medicine.
4. Web of Science - A citation indexing service that provides access to systematic reviews across various disciplines, including health sciences and ML.
5. Scopus - A large abstract and citation database of peer-reviewed literature, including systematic reviews on the use of ML in healthcare.
6. IEEE Xplore - A database for accessing the full text of IEEE transactions, journals, magazines, and conference proceedings, including systematic reviews on ML applications in biomedical engineering and healthcare.
7. EBSCO - A research platform that provides access to various databases, including systematic reviews on ML in health sciences.
The Problem, Indicator, Comparison, and Outcome (PICO) framework helped identify the most relevant keywords to use in the search. It ensures the search is focused on the most important aspects of the question and directly relevant results are selected. Therefore, a combination of keywords related to "machine learning", "artificial intelligence", "systematic review", " healthcare", “health science”, and “well-being” was used.
To ensure the validity and reliability of the findings, reduce bias in the selection of studies, and identify gaps in the literature, the following criteria were developed after the research question was finalized but before the search was carried out:
Inclusion Criteria (set the boundaries for the literature review):
• Specific study characteristics.
• Report characteristics (years considered, language, publication status).
• Method of research and reasoning.
• Availability of a relevant comparison in the study.
• Studies published within a specific time frame (last 4 years).
Exclusion Criteria (the elements that disqualify the study from inclusion in the literature review):
• The study used an inappropriate research design.
• The study had a limited wingspan.
• The study was published in a language other than English.
• The study was published more than 4 years ago.
Results and Discussion
Key points, ideas, and conclusions of the original literature
ML has become widely used in healthcare research due to its ability to process complex and high-dimensional data, such as genomics and electronic health records. Its algorithms can discover sophisticated patterns in these data sets that would be difficult to find using classical statistical methods. In addition, it has many applications, including diagnosis, treatment, and risk prediction6 7 8. Systematic literature reviews have identified over 10,000 ML algorithms used in healthcare, with the most common being neural networks, support vector machines, and random forests or decision trees9. The most frequent areas of ML application in healthcare are oncology and neurology, likely reflecting the prevalence of these diseases9. ML has demonstrated high predictive ability in many disease areas, but the reporting quality of these studies is often low, with many lacking data on accuracy, sensitivity, specificity, and validation9 10. The most used data source for ML in healthcare is radiological imaging, which has been used to develop ML solutions for clinical decision support9. Neural networks and deep learning are the most frequently published ML techniques, as they can detect complex nonlinear relationships in data9. While the potential of ML to improve healthcare outcomes is significant, the lack of rigorous assessment of ML performance in many studies is a concern that needs to be addressed to facilitate the widespread adoption of these technologies in healthcare settings9.
Main questions the literature attempts to address.
Overall, the literature on ML in health science underscores the importance of aligning values, addressing challenges, and leveraging the potential of ML to revolutionize healthcare11. The latter will be achieved by improving patient outcomes, reducing costs, and accelerating medical advancements while ensuring ethical and effective integration into the healthcare system. It explores how ML can boost healthcare through applications in medical imaging, clinical decision support, drug discovery, and electronic health records, while also addressing the challenges around data quality, privacy, and regulatory compliance12. The integration of ML and medicine is primarily aimed at enhancing the efficiency, accuracy, and personalization of healthcare rather than replacing doctors entirely. ML would improve the capabilities of medical professionals, allowing them to focus more on patient care and clinical judgment12.
Important points, evidence, and conclusions
The literature indicates that ML has significant potential to advance healthcare research by uncovering complex patterns in rich health data. However, the use of ML for individual patient care must be approached cautiously and meet the highest standards to address ethical concerns and ensure quality patient outcomes. Here is a selection of the important points discussed in the literature, with some details:
1. Applications of ML in healthcare: ML has been extensively used in healthcare for predictive analytics, event prediction, and improving health outcomes9 8. The literature emphasizes that ML algorithms, including neural networks, support vector machines, and random forest/decision trees, have been widely applied in healthcare settings9.
2. Disease areas and ML ability: The literature reveals that ML applications are prevalent in oncology and neurology, showcasing high prediction abilities in various disease areas9. ML algorithms, particularly artificial neural networks, and deep learning methods have been instrumental in enhancing sensitivity and specificity in radiographic studies9.
3. Data quality and validation: The literature points out the importance of data quality and validation in ML applications in healthcare. It highlights the need for improved reporting quality, especially in terms of accuracy, sensitivity, specificity, and validation methods for handling missing data9.
4. Future implications: The literature suggests that the digital revolution driven by ML is poised to transform the healthcare system significantly, leading to improved health outcomes and increased efficiency in healthcare delivery9. The potential of ML to revolutionize healthcare is underscored9.
To sum up, the literature underscores the transformative impact of ML on healthcare, particularly in disease prediction, treatment optimization, and medicine management. The evidence presented highlights the broad applications of ML algorithms in healthcare and the need for continued research and development to harness the full potential of ML in improving health outcomes.
ML has significantly contributed to health science research by enabling the analysis of complex data sets6 3 8. Its algorithms have been applied in various healthcare settings, including disease diagnosis, hospital management, and patient footfall management3 8. The increasing availability of data and computing power has made ML a viable approach to faster, more efficient healthcare delivery9. ML has been used to analyze data and predict the underlying causes of illnesses while employing disease-causing patterns and relationships3. The field of precision medicine has also seen significant applications of ML, using rich patient information to precisely target interventions6. ML has the potential to improve health outcomes and increase healthcare efficiency by analyzing massive datasets and extracting hidden information and patterns from them8 9.
Balanced discussion and evaluation of previous work
To base its critique on previous literature, this critical survey considered the following specific criteria:
1. Significance and contribution of each source to the field: Evaluate the literature aim, the achievement of that aim, the addition to the body of knowledge, the relationship to other works, and any missing aspects.
2. Methodology: Assess the research approach used, its objectivity or bias, the validity and reliability of results, and the analytical framework employed.
3. Argument and the use of evidence: Analyze the clarity of the hypothesis, the consistency of the argument, the types and effectiveness of evidence, and the justification of conclusions.
These criteria helped to evaluate and critique previous literature while ensuring comprehensive and insightful analysis.
Systematic reviews in healthcare identified over 10,000 ML algorithms used, with the most common being neural networks (2,454 algorithms), support vector machines (1,578), and random forest/decision trees (1,522)9.
The most frequent areas of ML application were oncology and neurology, likely reflecting the prevalence of these diseases and the potential of ML to aid in clinical prediction, categorization, and prognosis, especially using imaging data9.
However, the quality of reporting on these ML algorithms was poor, with many studies lacking data on accuracy (44%), sensitivity (72%), specificity (75%), internal (65%), and external validation (99%). Only 2% of studies reported a methodological approach for handling missing data9.
The review also found that the most used ML data source was radiological imaging. Deep learning methods were commonly applied in oncology and respiratory disease studies9.
Overall, the literature indicates significant potential for greater adoption of ML in healthcare, but the lack of rigorous assessment and reporting of these algorithms' performance needs to be addressed to facilitate their real-world application9.
Strengths of ML in healthcare
The reviewed literature provides a comprehensive overview of the current state of using ML in healthcare. It highlights several significant benefits, such as:
1. Improved predictive ability: ML algorithms have demonstrated high accuracy in predicting various health outcomes, such as disease diagnosis, treatment response, and risk assessment2. This can help medical professionals make better decisions.
2. Handling complex data: ML excels at processing and extracting insights from large, complex healthcare datasets, including medical images, electronic health records, and genomic data2. This can lead to a better understanding of disease patterns and personalized treatment approaches.
3. Automation and efficiency: ML can automate repetitive tasks, such as image analysis and patient monitoring, freeing healthcare professionals to focus on more complex clinical decision-making2.
4. Identification of emerging trends: ML can uncover emerging trends and patterns in health science, which can inform strategic management and guide future research priorities.
5. Improved decision-making: ML algorithms can assist in clinical decision-making by analyzing data to identify diseases, recommend treatments, and enhance patient care efficiency.
6. Reducing human errors: By automating routine tasks and data analysis, machine learning helps reduce the likelihood of human errors, leading to more accurate diagnoses and treatment plans.
7. Enhancing patient outcomes: ML applications in healthcare can streamline diagnostics, predict outcomes, and personalize treatment plans, ultimately improving patient outcomes.
8. Efficiency and cost-effectiveness: ML tools can automate tasks, streamline processes, and reduce operational costs, allowing healthcare professionals to focus more on patient care.
9. Innovative medical applications: ML enables personalized medicine, early disease detection, drug discovery, and robotic-assisted surgeries, contributing to advancements in healthcare technology and patient care.
10. Future growth potential: With the continuous advancements in ML, its adoption in healthcare is expected to expand further, offering more innovative solutions2.
These strengths highlight the transformative impact of ML in healthcare, paving the way for more efficient, accurate, and personalized practices.
Weaknesses and challenges
The literature also identifies several weaknesses and challenges in the application of ML in healthcare:
1. Lack of transparency and interpretability: Many ML models, particularly deep learning algorithms, are often considered "black boxes," making it difficult to understand the reasoning behind their predictions. This can hinder trust and acceptance among healthcare providers13 14.
2. Data quality and availability: The success of ML models is heavily dependent on the quality and availability of healthcare data, which can be limited or biased in certain settings13 14. Insufficient or biased data can lead to poor model performance13.
3. Ethical and regulatory concerns: The use of ML in healthcare raises important ethical and regulatory considerations, such as patient privacy, data security, and algorithmic bias, which need to be carefully addressed13 14.
4. Limited external validation: The literature review found that only a small percentage of studies reported external validation of their ML models, which is crucial for assessing their real-world performance and generalizability14.
5. Bias in algorithms: ML algorithms can be biased if the training data used to develop them is not representative or contains inherent biases. This can lead to inaccurate diagnoses or treatment recommendations that discriminate against certain patient populations.
6. Need for human oversight: While machine learning can automate many tasks, it still requires human supervision and verification, especially when dealing with critical medical decisions that impact patient lives.
7. Potential for security and privacy risks: The use of patient data for ML raises concerns about data privacy and the risk of cyberattacks compromising sensitive medical information14.
8. Inability to account for social factors: ML models may not be able to fully capture the complex social, economic, and environmental factors that can influence health outcomes for individual patients14.
9. Risk of job displacement: The automation of certain medical tasks through ML could potentially lead to job losses for healthcare workers, which need to be carefully managed.
In summary, while ML holds great promise for improving healthcare, there are significant challenges around bias, interpretability, data quality, privacy, and social factors that must be addressed to realize its full potential safely and ethically.
Notable Features
The literature review also highlights several notable features of the current state of ML in healthcare:
1. Predominance of neural networks: The most used ML algorithms in healthcare are artificial neural networks, including deep learning methods, which have shown impressive performance in areas like medical imaging and disease prediction9.
2. Oncology and neurology dominance: The review found that oncology and neurology were the most frequently studied disease areas in the identified systematic literature reviews, reflecting the significant interest and potential of ML in these domains9.
3. Lack of reporting quality: The review identified a concerning lack of reporting quality in many studies, with a significant proportion failing to provide crucial information about model accuracy, sensitivity, specificity, and validation procedures9.
4. Growing popularity: ML is becoming increasingly popular in health science research due to the proliferation of complex or unstructured data sets and the increased capacity and access to computing power needed to run these models.
5.; Diverse applications: ML is being applied in various healthcare sectors, including medicine, nursing, biochemistry, health professions, immunology, pharmacology, toxicology, and many more.
6. Methodological advancements: The literature highlights the development of new ML methodologies, such as probabilistic ML and deep learning approaches, which are being used to improve the accuracy and efficiency of ML models in healthcare.
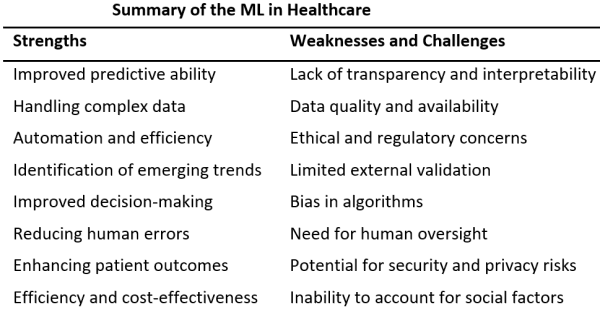
Overall, as illustrated in Table 1, the literature review presents a balanced assessment of the strengths, weaknesses, and notable features of the current state of ML in healthcare. While ML has demonstrated significant potential to improve healthcare outcomes and strategic management, there are still important challenges and limitations that need to be addressed to facilitate widespread adoption and trust in these technologies.
|
Strengths |
Weaknesses and Challenges |
Notable Features and Perspectives |
|
Improved predictive ability |
Lack of transparency and interpretability |
Predominance of neural networks |
|
Handling complex data |
Data quality and availability |
Oncology and neurology dominance |
|
Automation and efficiency |
Ethical and regulatory concerns |
Lack of reporting quality |
|
Identification of emerging trends |
Limited external validation |
Growing popularity |
|
Improved decision-making |
Bias in algorithms |
Diverse applications |
|
Reducing human errors |
Need for human oversight |
Methodological advancements |
|
Enhancing patient outcomes |
Potential for security and privacy risks |
|
|
Efficiency and cost-effectiveness |
Inability to account for social factors |
|
|
Innovative medical applications |
Risk of job displacement |
|
|
Future growth potential |
|
|
Table 1: Summary of the ML in Healthcare
Takeaway points and research gaps
Machine learning in healthcare is revolutionizing the industry with its transformative capabilities. Here are some key takeaway points about machine learning in healthcare:
• Applications: ML is used in various healthcare applications such as predicting and treating diseases, providing medical imaging and diagnostics, discovering, and developing new drugs, and organizing medical records.
• Benefits: The benefits of ML in healthcare include faster data collection, accelerated drug discovery and development, cost-efficient processes, and personalized treatment.
• Use Cases: ML is applied in healthcare for automating medical billing, clinical decision support, and developing clinical practice guidelines. It is also used to predict patient outcomes and assist in diagnosing diseases from imaging scans.
• Future Outlook: While ML enhances diagnostic accuracy and treatment personalization, it is unlikely to replace doctors entirely. Instead, it serves as a valuable ally, improving patient outcomes and allowing healthcare professionals to focus on patient care and clinical judgment.
These points highlight the significant role machine learning plays in advancing healthcare by improving patient care, diagnosis, treatment, and operational efficiency. However, the research gaps on machine learning in healthcare revolve around the challenges of effectively implementing AI-enabled tools, addressing the disconnect between model development and deployment, ensuring actionability, safety, and utility of algorithms, and developing best practices for monitoring, updating, and maintaining prediction models in clinical environments.
Limitations
The limitations of this critical review encompass various aspects that might impact the review process and its outcomes. These limitations include factors such as the lack of domain-specific expertise (Health Science), the necessity of human expertise, contextual understanding, and critical thinking skills in conducting thorough and insightful evaluations of research work in both domains of discourse (Computer Science -AI- and Healthcare).
Conclusion
The overall opinion of the literature ascertains that ML has significant potential to transform health science holistically and healthcare particularly. However, its integration into the latter requires careful consideration of important values and ethical concerns. While ML can automate certain tasks and provide more personalized care, there are risks of encoding societal biases and compromising patient autonomy if not implemented thoughtfully. Commercialization of ML healthcare products can also conflict with open and ethical research practices. Researchers must deliberate on the values underlying ML for healthcare, such as respect for persons, beneficence, and non-maleficence, and find ways to merge these with the core values of ML, like openness and reproducibility.
Overall, continued interdisciplinary collaboration and value-driven innovation will be key to realizing the full potential of ML in the medical field. Incidentally, here are some further recommendations to be considered:
1. Focus on specific health science fields.
2. Address risks and challenges: acknowledge and address the risks and challenges associated with ML applications in health science, such as system privacy and ethical concerns. It is crucial to develop strategies to mitigate these challenges for the successful integration of ML in health science settings.
3. Boost collaboration within healthcare to develop common databases for open-source ML models, particularly using medical imaging.
Conflict of Interest: the author states that no conflict of interest exists.
References
1 Rusinovich Y. Why "ML in Health Science". Web3MLHS. 2024;1(1). doi:10.62487/e4ccm968.
2 Habehh H, Gohel S. Machine Learning in Healthcare. Curr Genomics. 2021;22(4):291-300. doi:10.2174/1389202922666210705124359.
3 An Q, Rahman S, Zhou J, Kang JJ. A Comprehensive Review on Machine Learning in Healthcare Industry: Classification, Restrictions, Opportunities and Challenges. Sensors (Basel). 2023;23(9). doi:10.3390/s23094178.
4 Chen IY, Pierson E, Rose S, Joshi S, Ferryman K, Ghassemi M. Ethical Machine Learning in Healthcare. Annu Rev Biomed Data Sci. 2021;4:123-144. doi:10.1146/annurev-biodatasci-092820-114757.
5 Ciobanu-Caraus O, Aicher A, Kernbach JM, Regli L, Serra C, Staartjes VE. A critical moment in machine learning in medicine: on reproducible and interpretable learning. Acta Neurochir (Wien). 2024;166(1):14. doi:10.1007/s00701-024-05892-8.
6 Cho H, She J, Marchi D de, et al. Machine Learning and Health Science Research: Tutorial. J Med Internet Res. 2024;26:e50890. doi:10.2196/50890.
7 Ali O, Abdelbaki W, Shrestha A, Elbasi E, Alryalat MAA, Dwivedi YK. A systematic literature review of artificial intelligence in the healthcare sector: Benefits, challenges, methodologies, and functionalities. Journal of Innovation & Knowledge. 2023;8(1):100333. doi:10.1016/j.jik.2023.100333.
8 Salhout SM. Machine learning in healthcare strategic management: a systematic literature review. AGJSR. 2023. doi:10.1108/AGJSR-06-2023-0252.
9 Kolasa K, Admassu B, Hołownia-Voloskova M, Kędzior KJ, Poirrier J-E, Perni S. Systematic reviews of machine learning in healthcare: a literature review. Expert Rev Pharmacoecon Outcomes Res. 2024;24(1):63-115. doi:10.1080/14737167.2023.2279107.
10 Baqraf YKA, Keikhosrokiani P, Al-Rawashdeh M. Evaluating online health information quality using machine learning and deep learning: A systematic literature review. Digit Health. 2023;9:20552076231212296. doi:10.1177/20552076231212296.
11 Ghassemi M, Mohamed S. Machine learning and health need better values. NPJ Digit Med. 2022;5(1):51. doi:10.1038/s41746-022-00595-9.
12 Tolsgaard MG, Boscardin CK, Park YS, Cuddy MM, Sebok-Syer SS. The role of data science and machine learning in Health Professions Education: practical applications, theoretical contributions, and epistemic beliefs. Adv Health Sci Educ Theory Pract. 2020;25(5):1057-1086. doi:10.1007/s10459-020-10009-8.
13 Khan B, Fatima H, Qureshi A, et al. Drawbacks of Artificial Intelligence and Their Potential Solutions in the Healthcare Sector. Biomed Mater Devices. 2023:1-8. doi:10.1007/s44174-023-00063-2.
14 Paiste HJ, Godwin RC, Smith AD, Berkowitz DE, Melvin RL. Strengths-weaknesses-opportunities-threats analysis of artificial intelligence in anesthesiology and perioperative medicine. Front Digit Health. 2024;6:1316931. doi:10.3389/fdgth.2024.1316931.
References
Rusinovich Y. Why "ML in Health Science". Web3MLHS. 2024;1(1). DOI: https://doi.org/10.62487/e4ccm968
Habehh H, Gohel S. Machine Learning in Healthcare. Curr Genomics. 2021;22(4):291-300. DOI: https://doi.org/10.2174/1389202922666210705124359
An Q, Rahman S, Zhou J, Kang JJ. A Comprehensive Review on Machine Learning in Healthcare Industry: Classification, Restrictions, Opportunities and Challenges. Sensors (Basel). 2023;23(9). DOI: https://doi.org/10.3390/s23094178
Ciobanu-Caraus O, Aicher A, Kernbach JM, Regli L, Serra C, Staartjes VE. A critical moment in machine learning in medicine: on reproducible and interpretable learning. Acta Neurochir (Wien). 2024;166(1):14. DOI: https://doi.org/10.1007/s00701-024-05892-8
Chen IY, Pierson E, Rose S, Joshi S, Ferryman K, Ghassemi M. Ethical Machine Learning in Healthcare. Annu Rev Biomed Data Sci. 2021;4:123-144. DOI: https://doi.org/10.1146/annurev-biodatasci-092820-114757
Salhout SM. Machine learning in healthcare strategic management: a systematic literature review. AGJSR. 2023. DOI: https://doi.org/10.1108/AGJSR-06-2023-0252
Ali O, Abdelbaki W, Shrestha A, Elbasi E, Alryalat MAA, Dwivedi YK. A systematic literature review of artificial intelligence in the healthcare sector: Benefits, challenges, methodologies, and functionalities. Journal of Innovation & Knowledge. 2023;8(1):100333. DOI: https://doi.org/10.1016/j.jik.2023.100333
Cho H, She J, Marchi D de, et al. Machine Learning and Health Science Research: Tutorial. J Med Internet Res. 2024;26:e50890. DOI: https://doi.org/10.2196/50890
Kolasa K, Admassu B, Hołownia-Voloskova M, Kędzior KJ, Poirrier J-E, Perni S. Systematic reviews of machine learning in healthcare: a literature review. Expert Rev Pharmacoecon Outcomes Res. 2024;24(1):63-115. DOI: https://doi.org/10.1080/14737167.2023.2279107
Baqraf YKA, Keikhosrokiani P, Al-Rawashdeh M. Evaluating online health information quality using machine learning and deep learning: A systematic literature review. Digit Health. 2023;9:20552076231212296. DOI: https://doi.org/10.1177/20552076231212296
Ghassemi M, Mohamed S. Machine learning and health need better values. NPJ Digit Med. 2022;5(1):51. DOI: https://doi.org/10.1038/s41746-022-00595-9
Tolsgaard MG, Boscardin CK, Park YS, Cuddy MM, Sebok-Syer SS. The role of data science and machine learning in Health Professions Education: practical applications, theoretical contributions, and epistemic beliefs. Adv Health Sci Educ Theory Pract. 2020;25(5):1057-1086. DOI: https://doi.org/10.1007/s10459-020-10009-8
Paiste HJ, Godwin RC, Smith AD, Berkowitz DE, Melvin RL. Strengths-weaknesses-opportunities-threats analysis of artificial intelligence in anesthesiology and perioperative medicine. Front Digit Health. 2024;6:1316931. DOI: https://doi.org/10.3389/fdgth.2024.1316931
Khan B, Fatima H, Qureshi A, et al. Drawbacks of Artificial Intelligence and Their Potential Solutions in the Healthcare Sector. Biomed Mater Devices. 2023:1-8. DOI: https://doi.org/10.1007/s44174-023-00063-2
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Neji Hasni (Author)

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.





Add a Comment:
Comments:
Article views: 0