Confounders in Predictive Medical Models: The Role of Religion
DOI:
https://doi.org/10.62487/2rm68r13Keywords:
Human-Centered AI, Healthcare Survey, Biased Predictor, Confounder, Dirty ConfoundersAbstract
Aim: The aim of this study was to assess the acceptance among natural science specialists of the current official regulatory recommendations to avoid utilizing artificial intelligence (AI) and machine learning (ML) models that could exacerbate social disparities. Materials and Methods: An anonymous online survey was conducted using the Telegram platform, where participants were asked a single question: "Do you consider the inclusion of religious status in AI and ML models justified from the perspective of medical ethics and science?" Respondents were provided with only two response options: "Yes" or "No." This survey was specifically targeted at international groups, focusing primarily on English and Russian-speaking clinicians and scientific researchers. Results: 134 unique individuals participated in the survey. The results revealed that two-thirds of the respondents (87 individuals) agreed that including Religion status as predictor in the ML and AI models is inappropriate. Conclusion: Two-thirds of healthcare practitioners and scientific researchers participating in this survey agree that categorizing individuals within healthcare settings based on their religion is inappropriate. Constructing healthcare predictive models based on confounders like religion is unlikely to aid in identifying or treating any pathology or disease. However, the high conflict potential of this predictor may deepen societal disparities.
Do you consider the inclusion of religious status in artificial intelligence and machine learning models justified from the perspective of medical ethics and science?
Results:
Original Article
Background
Religion as Confounder in Machine Learning
Religion is a strong belief in a higher, unseen controlling power1. The research question is: Can this parameter of an individual's perception of the world around them be incorporated into machine learning (ML) models within healthcare and natural science settings? The evidence suggesting that this parameter can potentially predict some physiological or pathophysiological conditions is highly discrepant and inhomogeneous. However, the most compelling explanation for the role of religion in predictive modeling is that a religious group should be viewed as a community of people who share not only religious beliefs but also similarities in socio-economic, ethnic, and cultural backgrounds2. This implies that behind the concept of religion lie various factors such as diet, behaviors, geographic region, and social income, among others, since the strength of belief and religious perception is highly individual.
Employing religion in ML models, especially in public health settings, can introduce bias and categorize people based on a factor with confounding and conflict potential3. Numerous studies indicate that the inclusion of this predictor can harm physical and mental health due to increased social disparities4 5 6 7 8 9 10.
Aim
The aim of this study was to assess the acceptance among natural science specialists of the current official regulatory recommendations to avoid utilizing artificial intelligence (AI) and machine learning (ML) models that could exacerbate social disparities11 3. Specifically, this research investigated the role of religion in AI and ML models within healthcare settings.
Material and Methods
An anonymous online survey was conducted using the Telegram platform, where participants were asked a single question: "Do you consider the inclusion of Religious status in Artificial Intelligence and Machine Learning models justified from the perspective of medical ethics and science?” Respondents were provided with only two response options: "Yes" or "No."
The survey was targeted at international groups, focusing primarily on Russian and English-speaking clinicians and scientific researchers.
Statistics
The collected data were analyzed using descriptive statistics to interpret the responses.
Results
The survey was conducted in January-February 2024 with 134 unique and verified individuals participating. The results revealed that 2/3 of the respondents (87 individuals) agreed that including religion status as predictor in the current ML and AI models is inappropriate.
The results of this survey are openly accessible on the official Telegram Channel of the Web3 Society: ML in Health Science, which can be found at: https://t.me/MLinHS
Table 1 and Figure 1 summarize the survey results:
|
Variable |
Respondents |
|
Yes |
47 |
|
No |
87 |
|
Total |
134 |
Table 1: Do you consider the inclusion of religious status in artificial intelligence and machine learning models justified from the perspective of medical ethics and science?
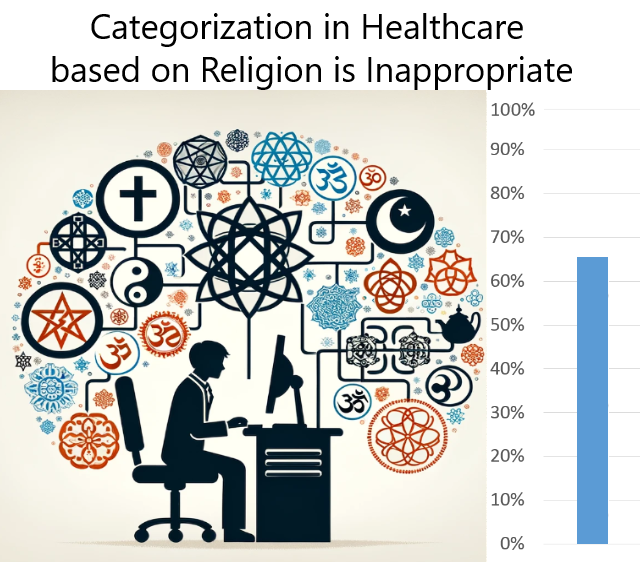
Figure 1: Survey Results. DALL E.
Discussion
Practical standpoint
Our findings indicate a high level of understanding among healthcare practitioners and scientific researchers regarding the role of religion as a confounder in ML and AI models within healthcare settings. This becomes even more apparent when comparing these results with the acceptance of nationality as a confounder, where only one-third acknowledge the inappropriateness of this predictor12. However, the overall acceptance of contemporary official regulators' recommendations falls short of the ideal 100% agreement.
AI and ML models cannot distinguish individual human characteristics. Consequently, constructing subgroups based on confounders like religion and nationality is unlikely to address the true causes of pathology or disease. However, the high conflict potential of these predictors may exacerbate societal disparities.
Limitations
The main limitation of this study was its reliance on anonymous survey methodology, which introduces potential bias in the purity of the cohort. Additionally, the limited number of participants represents another significant constraint.
To the best of our knowledge, this is the inaugural study to explore perspectives on incorporating the predictor religion into ML and AI models within healthcare settings.
Conclusion
Two-thirds of healthcare practitioners and scientific researchers participating in this survey agree that categorizing individuals within healthcare settings based on their religion is inappropriate. Constructing healthcare predictive models based on confounders like religion is unlikely to aid in identifying or treating any pathology or disease. However, the high conflict potential of this predictor may deepen societal disparities.
Conflict of Interest: YR and VR state that no conflict of interest exists.
Authorship: YR: Concept, data analysis, original draft, survey. YR, VR: Review and editing.
References
1 Behere PB, Das A, Yadav R, Behere AP. Religion and mental health. Indian J Psychiatry. 2013;55(Suppl 2):S187-94. doi:10.4103/0019-5545.105526.
2 Schlundt DG, Franklin MD, Patel K, et al. Religious affiliation, health behaviors and outcomes: Nashville REACH 2010. Am J Health Behav. 2008;32(6):714-724. doi:10.5555/ajhb.2008.32.6.714.
3 European Parliamentary Research Service. Artificial intelligence act. link.
4 Sharif MZ, Truong M, Alam O, et al. The association between experiences of religious discrimination, social-emotional and sleep outcomes among youth in Australia. SSM Popul Health. 2021;15:100883. doi:10.1016/j.ssmph.2021.100883.
5 Wu Z, Schimmele CM. Perceived religious discrimination and mental health. Ethn Health. 2021;26(7):963-980. doi:10.1080/13557858.2019.1620176.
6 Jordanova V, Crawford MJ, McManus S, Bebbington P, Brugha T. Religious discrimination and common mental disorders in England: a nationally representative population-based study. Soc Psychiatry Psychiatr Epidemiol. 2015;50(11):1723-1729. doi:10.1007/s00127-015-1110-6.
7 Baqai B, Azam L, Davila O, Murrar S, Padela AI. Religious Identity Discrimination in the Physician Workforce: Insights from Two National Studies of Muslim Clinicians in the US. J Gen Intern Med. 2023;38(5):1167-1174. doi:10.1007/s11606-022-07923-5.
8 Bender M, van Osch Y, He J, Güngör D, Eldja A. The role of perceived discrimination in linking religious practices and well-being: A study among Muslim Afghan refugees in the Netherlands. Int J Psychol. 2022;57(4):445-455. doi:10.1002/ijop.12854.
9 Alsubaie MK, Dolezal M, Sheikh IS, et al. Religious coping, perceived discrimination, and posttraumatic growth in an international sample of forcibly displaced Muslims. Ment Health Relig Cult. 2021;24(9):976-992. doi:10.1080/13674676.2021.1973978.
10 Scheitle CP, Frost J, Ecklund EH. The Association between Religious Discrimination and Health: Disaggregating by Types of Discrimination Experiences, Religious Tradition, and Forms of Health. Scientific Study of Religion. 2023;62(4):845-868. doi:10.1111/jssr.12871.
11 World Health Organization, ed. Ethics and governance of artificial intelligence for health: Guidance on large multi-modal models; 2024. link.
12 Rusinovich Y, Rusinovich V. Confounders in Predictive Medical Models: Roles of Nationality and Immigrant Status. Web3MLHS. 2024;1(1). doi:10.62487/vc54ms96.
References
Behere PB, Das A, Yadav R, Behere AP. Religion and mental health. Indian J Psychiatry. 2013;55(Suppl 2):S187-94. doi:10.4103/0019-5545.105526. DOI: https://doi.org/10.4103/0019-5545.105526
Schlundt DG, Franklin MD, Patel K, et al. Religious affiliation, health behaviors and outcomes: Nashville REACH 2010. Am J Health Behav. 2008;32(6):714-724. doi:10.5555/ajhb.2008.32.6.714. DOI: https://doi.org/10.5993/AJHB.32.6.15
European Parliamentary Research Service. Artificial intelligence act. https://www.europarl.europa.eu/RegData/etudes/BRIE/2021/698792/EPRS_BRI(2021)698792_EN.pdf.
Sharif MZ, Truong M, Alam O, et al. The association between experiences of religious discrimination, social-emotional and sleep outcomes among youth in Australia. SSM Popul Health. 2021;15:100883. doi:10.1016/j.ssmph.2021.100883. DOI: https://doi.org/10.1016/j.ssmph.2021.100883
Wu Z, Schimmele CM. Perceived religious discrimination and mental health. Ethn Health. 2021;26(7):963-980. doi:10.1080/13557858.2019.1620176. DOI: https://doi.org/10.1080/13557858.2019.1620176
Jordanova V, Crawford MJ, McManus S, Bebbington P, Brugha T. Religious discrimination and common mental disorders in England: a nationally representative population-based study. Soc Psychiatry Psychiatr Epidemiol. 2015;50(11):1723-1729. doi:10.1007/s00127-015-1110-6. DOI: https://doi.org/10.1007/s00127-015-1110-6
Baqai B, Azam L, Davila O, Murrar S, Padela AI. Religious Identity Discrimination in the Physician Workforce: Insights from Two National Studies of Muslim Clinicians in the US. J Gen Intern Med. 2023;38(5):1167-1174. doi:10.1007/s11606-022-07923-5. DOI: https://doi.org/10.1007/s11606-022-07923-5
Bender M, van Osch Y, He J, Güngör D, Eldja A. The role of perceived discrimination in linking religious practices and well-being: A study among Muslim Afghan refugees in the Netherlands. Int J Psychol. 2022;57(4):445-455. doi:10.1002/ijop.12854. DOI: https://doi.org/10.1002/ijop.12854
Alsubaie MK, Dolezal M, Sheikh IS, et al. Religious coping, perceived discrimination, and posttraumatic growth in an international sample of forcibly displaced Muslims. Ment Health Relig Cult. 2021;24(9):976-992. doi:10.1080/13674676.2021.1973978. DOI: https://doi.org/10.1080/13674676.2021.1973978
Scheitle CP, Frost J, Ecklund EH. The Association between Religious Discrimination and Health: Disaggregating by Types of Discrimination Experiences, Religious Tradition, and Forms of Health. Scientific Study of Religion. 2023;62(4):845-868. doi:10.1111/jssr.12871. DOI: https://doi.org/10.1111/jssr.12871
World Health Organization, ed. Ethics and governance of artificial intelligence for health: Guidance on large multimodal models; 2024.
Rusinovich Y, Rusinovich V. Confounders in Predictive Medical Models: Roles of Nationality and Immigrant Status. Web3MLHS. 2024;1(1). doi:10.62487/vc54ms96. DOI: https://doi.org/10.62487/vc54ms96
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Yury Rusinovich, Volha Rusinovich (Author)

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.





Add a Comment:
Comments:
Article views: 0